Aspirin Could Help Reduce HIV Infections In Women -- A Dramatic, Promising Research Result In Nairobi
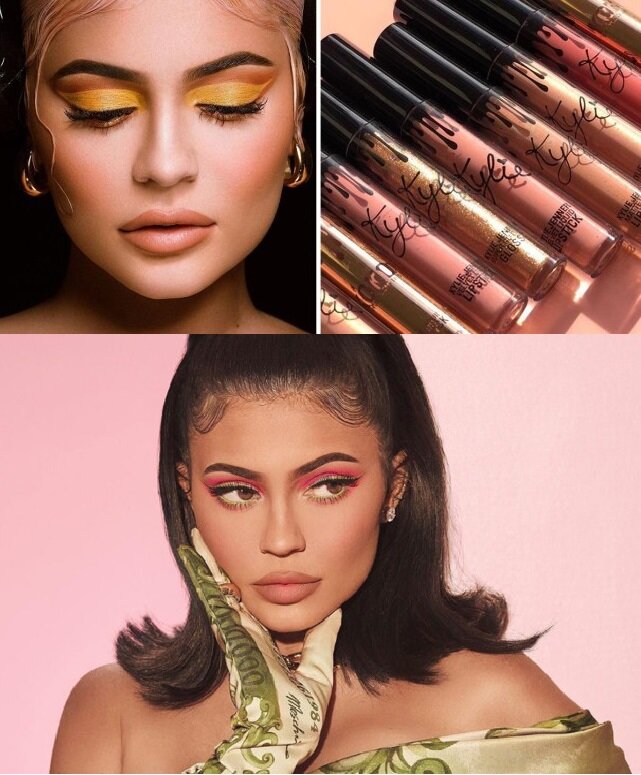
/Women in Kenya. Photo by John McArthur on Unsplash
By Colin Graydon, PhD Candidate in Medical Microbiology, University of Manitoba and Monika Kowatsch PhD Student in Medical Microbiology, University of Manitoba. First published on The Conversation Africa.
With nearly two million new infections and one million associated deaths each year, the HIV (human immunodeficiency virus) pandemic is alive and well. Thirty-seven million people are now living with HIV, more than half of whom are women.
Today, most HIV transmission occurs through sex. Fortunately, you can protect yourself and others by keeping HIV away (abstinence, condom use, circumcision) or by inactivating HIV (microbicide gels or a combination of prophylactic anti-HIV drugs such as PrEP). However, these methods are not always feasible for many and can come with stigma.
Imagine though, if instead of targeting the virus, we could make people less susceptible to HIV and address the needs of communities by using a relatively safe, affordable and globally accessible drug with no associated stigma. This is where Aspirin comes in.
It may sound like a fairy tale, but results from our lab’s pilot study published last monthsuggest it may be true. Plus, there’s good science behind the explanation.
Aspirin reduced HIV ‘target cells’
The idea comes from a partnership with a community of women in Nairobi, Kenya over more than 30 years. This relationship has led to establishment of a clinic which provides almost 50,000 sex workers with disease prevention and treatment resources, and is often referred to by the WHO and UNAIDS as a model of best practices.
Remarkably, many of these women are naturally resistant to HIV, at least in part because they have very little inflammation in their blood and genital tract. This is important because inflammation can increase HIV infection by 1) recruiting immune cells to the site of inflammation, including the cells that HIV loves to infect — so-called HIV “target cells” and 2) activating these HIV target cells, which increases their susceptibility to viral infection and enhances HIV’s ability to replicate within them.
The major question posed by our study was this: as an anti-inflammatory drug, could Aspirin reduce the number of HIV target cells and make them less activated?
To answer this question, our lab quantified HIV target cells in the blood and vagina of 37 Kenyan women before and after taking Aspirin for up to six weeks.
The results, published in the Journal of the International AIDS Society, show that aspirin reduced the frequency of vaginal HIV target cells by approximately 35 per cent and made them less activated.
As a bonus, Aspirin seemed to increase the structural integrity of the skin in the vagina, which could also prevent HIV infection by further restricting HIV’s access to more target cells in the blood.
We also tried another anti-inflammatory drug called hydroxychloroquine (HCQ). HCQ is less well known than Aspirin, but used to be a popular treatment for malaria and is now used to treat autoimmune diseases such as rheumatoid arthritis. HCQ also seemed to reduce inflammation in the vagina, but in a slightly different manner.
First drug to target the host
PrEP (a daily treatment of anti-HIV drugs used for prevention) is often used in the form of a vaginal gel, but does not work for women who have genital inflammation.
The next step will be a clinical trial testing whether Aspirin can reduce inflammation in women using PrEP and thereby reduce the number of HIV infections in women at high risk for HIV, such as female sex workers. This population has been asking about future research plans focusing on using Aspirin to prevent HIV.
If we can demonstrate this, Aspirin would be the first drug that targets the host, rather than the virus, to prevent HIV.
By acting on the host rather than the virus, Aspirin is not prone to generate HIV resistance, since there is no selective pressure for HIV to evolve around.
We are not yet at the stage where Aspirin can be recommended for preventing HIV, but the potential for another tool in our belt against a virus that has killed 35 million people (almost the population of Canada), can only be good news. Especially one as safe, affordable, accessible and non-stigmatizing as Aspirin.
Related: